Artificial intelligence (AI) has the potential to transform how healthcare is delivered. It can increase productivity and the efficiency of care delivery and allow healthcare systems to provide more and better care to more people. AI can help improve the experience of healthcare practitioners, enabling them to spend more time in direct patient care and reducing burnout.
Recently, artificial intelligence and machine learning have been revolutionizing the landscape of healthcare research and personalized precision medicine. There are now great volumes of health data, including patient medical records that have been made available through wearable sensors, health insurance claims, medical imaging, surveillance, and more. With the increasing advancement in hardware components, the rapid progress of machine learning algorithms (primarily using deep learning methods to analyze clinical data) is gradually having the following effects: enabling doctors to better diagnose; facilitating early disease detection; uncovering novel treatments and drug interactions; improving disease surveillance; and others. The development and research in this field are progressing faster than ever before.
Deep learning has shown remarkable success in the field of health informatics. However, due to the complex structure of the model, it remains still a black box, and demystifying this black box has become a major challenge. Significant research is needed for such issues and to address the development of methods for improved interpretability of machine learning predictions, reducing brittleness, and improving generalizability.
The aim of this Special Issue is to collect a wide variety of research into machine learning-based health informatics. Original research and review articles are welcomed.
Potential topics include but are not limited to the following:
- Management of digital healthcare and health informatics innovations
- An automated framework for disease diagnosis
- Early disease diagnosis and relevant treatment prediction
- AI-based pattern recognition methods
- AI-based Data and security management for Wearable medical devices
- Privacy and security in healthcare data management with A
- Deep learning for medical image processing and decision making
- Role and recent development of AI in Electronic Health Records
- AI and its applications in bioinformatics and computational biology
- AI-based cloud and data mining
Healthcare is one of the major success stories of our times. Medical science has improved rapidly, raising life expectancy around the world, but as longevity increases, healthcare systems face the growing demand for their services, rising costs and a workforce that is struggling to meet the needs of its patients.
Demand is driven by a combination of unstoppable forces: population ageing, changing patient expectations, a shift in lifestyle choices, and the never-ending cycle of innovation being but a few. Of these, the implications of an ageing population stand out. By 2050, one in four people in Europe and North America will be over the age of 65—this means the health systems will have to deal with more patients with complex needs. Managing such patients is expensive and requires systems to shift from an episodic care-based philosophy to one that is much more proactive and focused on long-term care management.
Healthcare spending is simply not keeping up. Without major structural and transformational change, healthcare systems will struggle to remain sustainable. Health systems also need a larger workforce, but although the global economy could create 40 million new health-sector jobs by 2030, there is still a projected shortfall of 9.9 million physicians, nurses and midwives globally over the same period, according to the World Health Organization.
Building on automation, artificial intelligence (AI) has the potential to revolutionize healthcare and help address some of the challenges set out above. There are several definitions of AI, but this report draws from a concise and helpful definition used by the European Parliament, “AI is the capability of a computer program to perform tasks or reasoning processes that we usually associate with intelligence in a human being.”
AI can lead to better care outcomes and improve the productivity and efficiency of care delivery. It can also improve the day-to-day life of healthcare practitioners, letting them spend more time looking after patients and in so doing, raise staff morale and improve retention. It can even get life-saving treatments to market faster. At the same time, questions have been raised about the impact AI could have on patients, practitioners, and health systems, and about its potential risks; there are ethical debates about how AI and the data that underpins it should be used.
AI in healthcare today
More data, better data, more connected data
What do we mean by AI in healthcare?
AI is now top-of-mind for healthcare decision-makers, governments, investors and innovators, and the European Union itself. An increasing number of governments have set out aspirations for AI in healthcare, in countries as diverse as Finland, Germany, the United Kingdom, Israel, China, and the United States and many are investing heavily in AI-related research. The private sector continues to play a significant role, with venture capital (VC) funding for the top 50 firms in healthcare-related AI reaching $8.5 billion, and big tech firms, startups, pharmaceutical and medical-devices firms and health insurers, all engaging with the nascent AI healthcare ecosystem.
Geographically, the dynamics of AI growth are shifting. The United States still dominates the list of firms with the highest VC funding in healthcare AI to date and has the most completed AI-related healthcare research studies and trials. But the fastest growth is emerging in Asia, especially China, where leading domestic conglomerates and tech players have consumer-focused healthcare AI offerings and Ping An’s Good Doctor, the leading online health-management platform already lists more than 300 million users. Europe, meanwhile, benefits from the vast troves of health data collected in national health systems and has significant strengths in terms of the number of research studies, established clusters of innovation and pan-European collaborations, a pan-European approach to core aspects of AI (e.g., ethics, privacy, “trustworthy AI”) and an emerging strategy on how to ensure the “EU way” for AI helps deliver the advantages for AI to its population. Yet, at the same time, valuable data sets are not linked, with critical data governance, access, and security issues still needing to be clarified, delaying further adoption. European investment and research in AI are strong when grouped together but fragmented at the country or regional level. Overall, there is a significant opportunity for EU health systems, but AI’s full potential remains to be explored and the impact on the ground remains limited. A surprising 44 per cent of the healthcare professionals we surveyed—and these were professionals chosen based on their engagement with healthcare innovation—had never been involved in the development or deployment of an AI solution in their organization.
Growing number of use cases
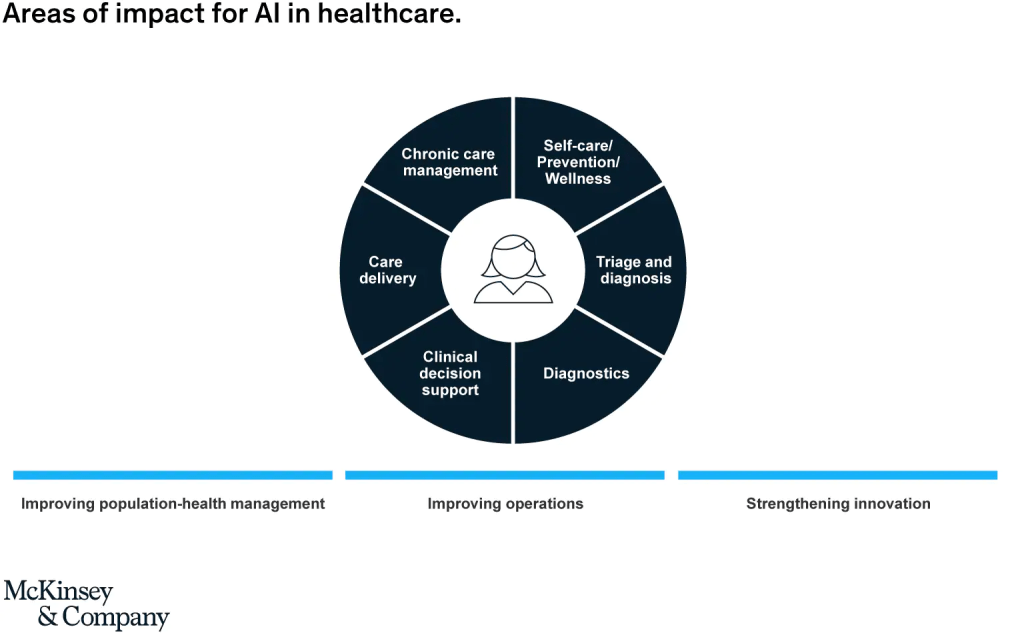
While there are widespread questions on what is real in AI in healthcare today, this report looked at 23 applications in use today and provides case studies of 14 applications already in use. These illustrate the full range of areas where AI can have impact: from apps that help patients manage their care themselves, to online symptom checkers and e-triage AI tools, to virtual agents that can carry out tasks in hospitals, to a bionic pancreas to help patients with diabetes. Some help improves healthcare operations by optimizing scheduling or bed management, others improve population health by predicting the risk of hospital admission or helping detect specific cancers early enabling intervention that can lead to better survival rates, and others even help optimize healthcare R&D and pharmacovigilance. The scale of many solutions remains small, but their increasing adoption at the health-system level indicates the pace of change is accelerating. In most cases, the question is less whether AI can have an impact, and more how to increase the potential for impact and, crucially, how to do so while improving the user experience and increasing user adoption.
Three phases of scaling AI in healthcare
We are in the very early days of our understanding of AI and its full potential in healthcare, in particular with regard to the impact of AI on personalization. Nevertheless, interviewees and survey respondents conclude that over time we could expect to see three phases of scaling AI in healthcare, looking at solutions already available and the pipeline of ideas.
First, solutions are likely to address the low-hanging fruit of routine, repetitive and largely administrative tasks, which absorb significant time of doctors and nurses, optimizing healthcare operations and increasing adoption. In this first phase, we would also include AI applications based on imaging, which are already in use in specialities such as radiology, pathology, and ophthalmology.
In the second phase, we expect more AI solutions that support the shift from hospital-based to home-based care, such as remote monitoring, AI-powered alerting systems, or virtual assistants, as patients take increasing ownership of their care. This phase could also include broader use of NLP solutions in the hospital and home setting, and more use of AI in a broader number of specialities, such as oncology, cardiology, or neurology, where advances are already being made. This will require AI to be embedded more extensively in clinical workflows, through the intensive engagement of professional bodies and providers. It will also require well-designed and integrated solutions to use existing technologies effectively in new contexts. This scaling up of AI deployment would be fuelled by a combination of technological advancements (e.g., in deep learning, NLP, connectivity etc.) and cultural change and capability building within organizations.
In the third phase, we would expect to see more AI solutions in clinical practice based on evidence from clinical trials, with an increasing focus on improved and scaled clinical decision-support (CDS) tools in a sector that has learned lessons from earlier attempts to introduce such tools into clinical practice and has adapted its mindset, culture and skills. Ultimately respondents would expect to see AI as an integral part of the healthcare value chain, from how we learn, to how we investigate and deliver care, to how we improve the health of populations. Important preconditions for AI to deliver its full potential in European healthcare will be the integration of broader data sets across organizations, strong governance to continuously improve data quality, and greater confidence from organizations, practitioners and patients in both the AI solutions and the ability to manage the related risks.
How will AI change the healthcare workforce?
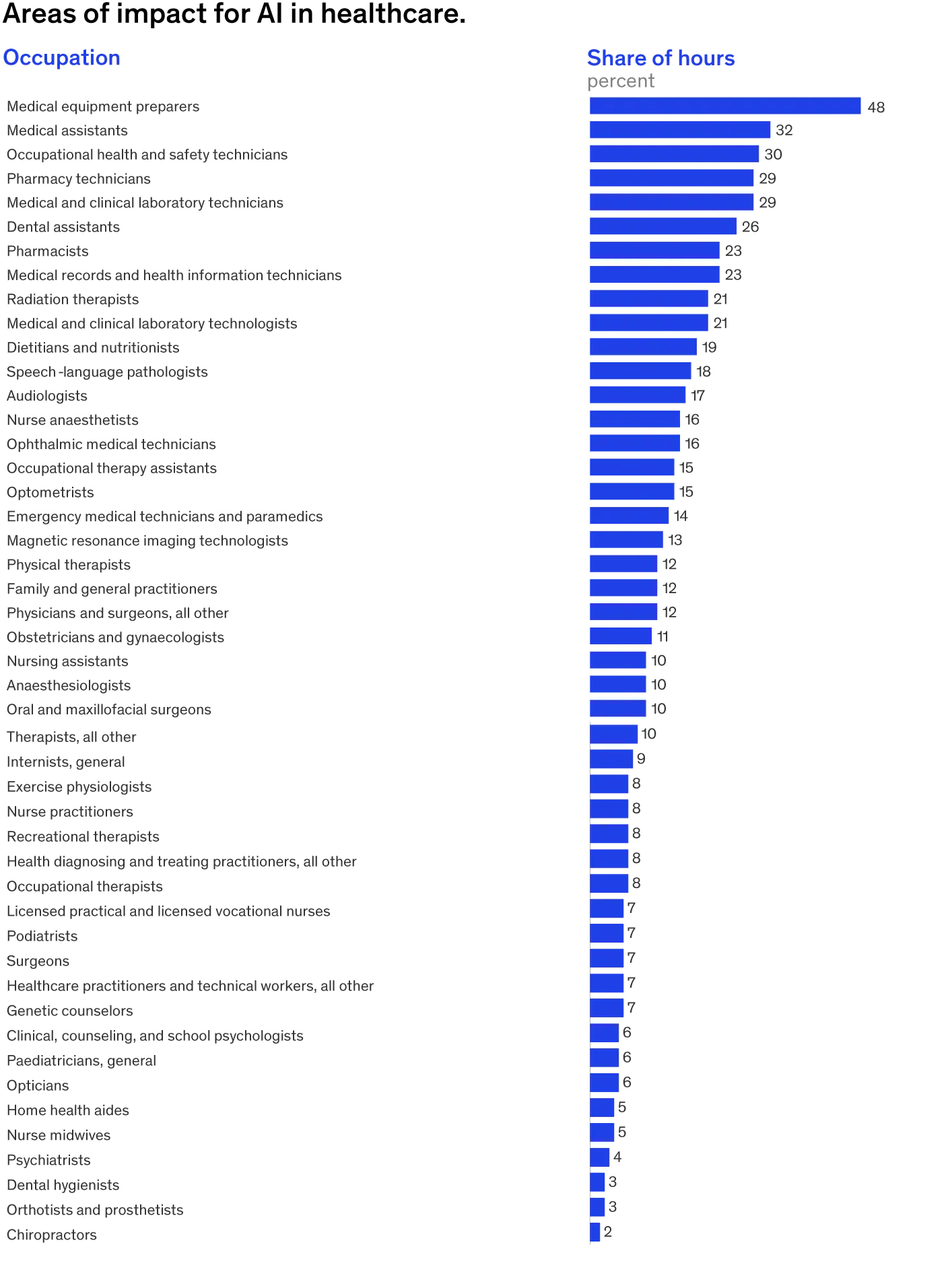
The MGI has studied how automation and AI are likely to affect the future of work. It concludes that automation will affect most jobs across sectors, but the degree varies significantly, and healthcare is one of the sectors with the lowest overall potential for automation—only 35 per cent of time spent is potentially automatable and this varies by type of occupation. The potential for automation is different to the likelihood of adoption.
The analysis uses a midpoint scenario, which estimates that 15 per cent of current work hours in healthcare are expected to be automated. Exhibit 2 shows the share of hours currently worked that could be freed up by automation by 2030 for a wide range of healthcare occupations in selected European countries. This does not reflect the potential for further disruption through other factors, such as personalization, that may revolutionize healthcare by focusing on a “segment of one.”
How will automation and AI affect the number of jobs in healthcare?
The reality is that the European healthcare sector faces a significant workforce gap that is only expected to widen. The World Health Organization estimates overall demand for healthcare workers to rise to 18.2 million across Europe by 2030 and, as an example, states that the current supply of 8.6 million nurses, midwives, and healthcare assistants across Europe will not meet current or projected future needs.
What needs to change to encourage the introduction and scaling of AI in healthcare?
The strides made in the field of AI in healthcare have been momentous. Moving to a world in which AI can deliver significant, consistent, and global improvements in care will be more challenging.
Of course, AI is not a panacea for healthcare systems, and it comes with strings attached. The analyses in this report and the latest views from stakeholders and frontline staff reveal a set of themes that all players in the healthcare ecosystem will need to address:
- Working together to deliver quality AI in healthcare. Quality came up in our interviews time and again, especially issues around the poor choice of use cases, AI design and ease of use, the quality and performance of algorithms, and the robustness and completeness of underlying data. The lack of multidisciplinary development and early involvement of healthcare staff and limited iteration by joint AI and healthcare teams were cited as major barriers to addressing quality issues early on and adopting solutions at scale. The survey revealed this is driven by both sides: only 14 per cent of startup executives felt that the input of healthcare professionals was critical in the early design phase; while the healthcare professionals saw the private sector’s role in areas such as aggregating or analyzing data, providing a secure space for data lakes, or helping upskill healthcare staff as minimal or nonexistent.
One problem AI solutions face is building clinical evidence of quality and effectiveness. While startups are interested in scaling solutions fast, healthcare practitioners must have proof that any new idea will “do no harm” before it comes anywhere near a patient. Practitioners also want to understand how it works, where the underlying data come from and what biases might be embedded in the algorithms, so are interested in going past the concept of AI as a “black box” to understand what underpins it. Transparency and collaboration between innovators and practitioners will be key in scaling AI in European healthcare.
User-centric design is another essential component of a quality product. Design should have the end user at its heart. This means AI should fit seamlessly with the workflow of decision-makers and by being used, it will be improved. Many interviewees agreed that if AI design delivers value to end users, those users are more likely to pay attention to the quality of data they contribute, thereby improving the AI and creating a virtuous circle. Finally, AI research needs to heavily emphasize explainable, causal, and ethical AI, which could be a key driver of adoption. - Rethinking education and skills. We have already touched on the importance of digital skills—these are not part of most practitioners’ arsenal today. AI in healthcare will require leaders well-versed in both biomedical and data science. There have been recent moves to train students in science where medicine, biology, and informatics meet through joint degrees, though this is less prevalent in Europe. More broadly, skills such as basic digital literacy, the fundamentals of genomics, AI, and machine learning need to become mainstream for all practitioners, supplemented by critical-thinking skills and the development of a continuous-learning mindset. Alongside upgrading clinical training, healthcare systems need to think about the existing workforce and provide ongoing learning, while practitioners need the time and incentive to continue learning.
- Strengthening data quality, governance, security and interoperability. Both interviewees and survey respondents emphasized that data access, quality, and availability were potential roadblocks. The data challenge breaks down into digitizing health to generate the data, collecting the data, and setting up governance around data management. MGI analyses show that healthcare is among the least digitized sectors in Europe, lagging behind in digital business processes, digital spending per worker, digital capital deepening, and the digitization of work and processes. It is critical to get the basic digitization of systems and data in place before embarking on AI deployments—not least because the frustrations staff have with basic digitization could spill over to the wider introduction of AI.
In addition, as more healthcare is delivered using new digital technologies, public concerns about how healthcare data are used have grown. Healthcare organizations should have robust and compliant data-sharing policies that support the improvements in care that AI offers while providing the right safeguards in a cost-efficient way. Physicians we interviewed emphasized that, given the volume of data required for AI, a poorly thought-out process of anonymization could be a major cost, making diagnostic algorithms prohibitively expensive.
Interviewees also emphasized, however, that both healthcare as a sector and Europe as a region have significant advantages. First, both healthcare organizations and health systems are used to dealing with sensitive data through well-structured data governance and risk-management processes. In some cases, healthcare could lead the way for other sectors seeking to put such measures in place. Secondly, Europe benefits from national health systems with extensive data sets, often shared within integrated care systems, offering a set of systems and processes to build on that could also serve as examples to other regions.
The final data challenge is getting data sets to talk to each other. Policymakers, funding bodies and nonprofit organizations need to support efforts to sufficiently anonymize and link data and, where sensible, to build databases that can be accessed by stakeholders with the appropriate safeguards. In order to make the most of the rich data that is available, healthcare systems need an interconnected data infrastructure. This is an area where Europe, as mentioned, could have a significant advantage, in terms of its extensive national data sets and its networks of innovations clusters or hubs and pan-European collaborations with academia and industry, providing a prototype for the creation of centres of excellence for AI in healthcare. - Managing change. Managing change while introducing AI is no different to managing change in complex institutions more broadly, but for healthcare, clinical leadership is key, as is being open to identifying the right use cases that support rather than antagonize practitioners and truly augment rather than substitute their ability to deliver the best possible care to their patients. This could include prioritizing solutions that focus on reducing the time people spend on routine administrative tasks, rather than those that seek to act as virtual assistants who interact directly with patients, or CDS tools that facilitate activities physicians see as core to their professional role, i.e., the clinical diagnosis.
Healthcare providers also need to be transparent about the benefits and risks of AI and work with staff to harness the collective energy of their teams and capitalize on the opportunities AI can bring. It may not be a rapid process, but it soon becomes increasingly rewarding for practitioners and is an important part of the overall adoption process. - Investing in new talent and creating new roles. Healthcare organizations need to consider how they will develop and recruit the new roles that will be critical to the successful introduction and adoption of AI, such as data scientists or data engineers. Demand for such skills is heating up across industries and the competition for talent will be fierce, but many young data professionals find a true vocation in healthcare and its mission and are excited about the potential of digital health and AI. Developing flexible, agile models to attract and retain such talent will be a key part of these organizations’ people strategy.
- Working at scale. The lessons from the public- and private-sector actors aiming to develop AI in healthcare to date suggest that scale matters—largely due to the resources needed to develop robust AI solutions or make them cost-efficient. Not every hospital will be able to afford to attract new AI talent or have access to enough data to make algorithms meaningful. Smaller organizations can benefit from working in innovation clusters that bring together AI, digital health, biomedical research, translational research or other relevant fields. Larger organizations can develop into centres of excellence that pave the way for regional and public-private collaborations to scale AI in European healthcare.
- Regulation, policymaking and liability, and managing risk. Responsibility for AI solutions—both clinical and technical—is split today between healthcare organizations and their staff. Interviewees emphasized the importance of clarifying whether AI will be regulated as a product or as a tool that supports decision-making, and of introducing a consistent regulatory approach for AI similar to that provided by the European Medicines Agency (EMA) on medicines or by national authorities on medical devices. Another issue to be clarified across Europe is the extent to which patients’ access to some AI tools needs to be regulated or restricted to prescription. The issue of liability and risk management is a particular challenge. Patient safety is paramount, but healthcare providers also have to think about the professional accountability of their clinicians, as well the protection of their organizations from reputational, legal or financial risk. Healthcare lawyers interviewed in this report were clear that accountability ultimately rests with the clinician under current laws. Innovators are also proactively addressing related risks. Many are putting new processes in place and ensuring a “compliance by design” approach is at the core of product development.
- Funding. The reimbursement of medicines and medical devices across Europe is complicated and is even less clear when it comes to AI solutions. The responsibility for decisions on the reimbursement of a medicine or device rests with national and local payor organizations depending on the country, and this decision usually covers what will be reimbursed and at what price. Clear criteria for the potential reimbursement of AI applications will be crucial for its adoption at scale, alongside creative funding models that ensure the benefits are shared across organizations.
What this could mean for healthcare organizations
European healthcare providers need to assess what their distinctive role or contribution can be in introducing or scaling AI in healthcare. They need to take stock of their capabilities, level of digitization, availability and quality of data, resources and skills and then define their level of ambition for AI as it fits with their strategic goals. They should also define the enablers they need to put in place. These could include creating an AI ecosystem through partnerships to codevelop the right solutions for their population; co-developing a compelling narrative on AI with patients and practitioners; defining and developing the right use cases jointly with end users; defining and addressing skill gaps in digital literacy for their staff; refining their value proposition for AI talent; addressing data-quality, access, governance, and interoperability issues; and shaping a culture of entrepreneurship. All these themes were echoed by the healthcare professionals in the survey, who listed the top three things healthcare organizations could do, such as bringing together multidisciplinary teams with the right skills, improving the quality and robustness of data and identifying the right use cases.
What this could mean for health systems
European health systems can play a more fundamental role in catalyzing the introduction and scaleup of AI. Key actions they could take include:
- Develop a regional or national AI strategy for healthcare, defining a medium- and longer-term vision and goals, specific initiatives, resources and performance indicators. Define use cases to support through targeted funding and incentives to enable scaling of AI solutions across the system; ensure these deliver against clinical and operational outcomes.
- Set standards for digitization, data quality and completeness, data access, governance, risk management, security and sharing, and system interoperability; incentivize adherence to standards through a combination of performance and financial incentives.
- Redesign workforce planning and clinical education processes to address the needs of both future healthcare and AI-focused professionals; and invest upfront in upskilling frontline staff and designing lifelong-learning programs through continuing professional development and degrees or diplomas for healthcare professionals.
- Provide incentives and guidance for healthcare organizations to collaborate in centres of excellence/clusters of innovation at the regional or national level.
- Address AI regulation, liability and funding issues, creating the right environment for appropriate, safe and effective AI solutions to be adopted but minimizing the risk to practitioners.
- Ensure this is reflected in funding and reimbursement mechanisms for innovation in healthcare—the number one priority for survey respondents from health systems, alongside simplifying data governance and data-sharing processes.

Leave a comment